
As parents, we will go the distance to protect our children’s health. We stay on top of their medical appointments, keep track of their milestones, and make sure they follow their vaccination schedules without missing a beat. But how often do we take a pause to think for ourselves? In a place like Singapore, where life moves quickly and there’s always something important on the schedule, it’s easy to put ourselves last — until something goes wrong.
This tendency to overlook our own needs often includes vaccinations. Most of us complete our routine childhood vaccines and rarely think about them again — and for good reason. Many of them offer long-term or lifelong protection. However, there are also vaccines that are recommended specifically for adults. These are not meant to replace earlier vaccines, but rather to address risks that emerge later in life — whether due to age, health conditions, lifestyle, or travel.
And because these vaccines are introduced later in life, they’re not always top of mind — especially when we feel fine and assume we’re already protected. But protection doesn’t always mean lifelong immunity, and that’s where it helps to think of your immune system like your smart device or computer. Every now and then, it needs an update to keep things running smoothly, and vaccinations are part of that update.
With that in mind, it’s worth taking stock of the vaccines you might need as an adult, understanding when they’re recommended, what they protect against, and why keeping them up to date is still an important part of staying healthy.
The Flu Vaccine – Why It’s Still a Good to Have
Influenza, or the flu, is a highly contagious respiratory infection that can cause symptoms like high fever, body aches, sore throat, blocked nose, and fatigue. In more serious cases, flu can lead to complications such as pneumonia, which in rare instances may result in death — even among otherwise healthy adults.
In Singapore, flu circulates year-round but tends to peak between April to July and November to January. During these periods, the virus spreads easily in schools, offices, crowded events, and on public transport.
Because of how quickly the bug spreads during these peak periods, a flu vaccination is important for reducing your risk. A flu shot will help you build protection against the season’s most common strains. While it might not prevent infection entirely, it can reduce the severity of symptoms and lower the chances of serious illness, hospitalisation, and long recovery periods.
Who Should Get the Flu Vaccine?
The flu vaccine is recommended for all adults, but is especially important for those who:
- Are aged 65 and above
- Are pregnant
- Have chronic conditions like diabetes, heart, kidney, or lung disease
- Have weakened immune systems
- Live with or care for infants, elderly parents, or those with higher health risks
How Often Should You Get the Flu Vaccine?
The flu virus mutates quickly, which means last year’s vaccine might not offer adequate protection against this year’s strains. New vaccines are developed and released annually to keep up with these changes. On top of that, your antibody levels may decline over time — another reason why an annual flu shot is recommended.
For some individuals with higher health risks, your doctor may advise getting it as often as every six months, depending on your condition and the current strains circulating.
The Pneumococcal Vaccine – Why It Shouldn’t Be Overlooked
Pneumococcal disease can lead to serious infections such as pneumonia, meningitis, bacteraemia, and ear infections. Although it is commonly associated with childhood, it continues to pose real risks to adults. The risk is especially higher for those aged 65 and above, or for individuals managing chronic conditions affecting the lungs, heart, kidneys, or immune system.
These infections don’t always begin in an obvious way. Symptoms can start with a mild cough, low-grade fever, or earache, and may be mistaken for something less serious. However, they have the potential to escalate into more severe signs such as chest pain, confusion, or intense headaches. Depending on how the infection spreads, complications may require hospitalisation and involve a longer recovery process.
While treatment is available, recovering from a serious pneumococcal infection can take time. It might involve prolonged discomfort, disruptions to daily life, and a longer-than-expected return to normal. In that sense, the price of not getting the vaccine can be far greater than many realise.
Who Should Get the Pneumococcal Vaccine?
In Singapore, the pneumococcal vaccine is recommended for adults aged 65 and above, as this group is more likely to experience serious complications. It is also advised for adults with long-term medical conditions such as diabetes, or chronic issues affecting the heart, lungs, kidneys, or liver. Individuals with weakened immune systems might also fall into a higher-risk group.
To offer protection against these risks, two types of pneumococcal vaccines are currently used. PCV13 (13-valent pneumococcal conjugate vaccine) protects against 13 common strains of the bacteria, while PPSV23 (23-valent pneumococcal polysaccharide vaccine) covers 23 strains.
How Often Should You Get the Pneumococcal Vaccine?
For most adults aged 65 and above, the typical schedule involves one dose of the PCV13 pneumococcal vaccine, followed by the PPSV23 pneumococcal vaccine at a later stage. This sequence helps build stronger and more lasting protection, especially in those who have never received either vaccine before.
If you’re below 65 but have certain medical conditions that increase your risk, your doctor may recommend starting earlier. The timing between doses may vary based on your health status and medical history, so it’s best to check with a healthcare provider to see what applies to you.

The Tdap Vaccine – Protection for Everyday Risks
Tetanus, diphtheria, and pertussis might seem like conditions from a different era, but they continue to pose real risks in adulthood. The Tdap vaccine — short for tetanus, diphtheria, and acellular pertussis — helps protect against all three. Starting with tetanus, this is a bacterial infection that enters the body through a cut, scrape, or puncture wound, often sustained from everyday activities at home or outdoors. Once inside the body, the bacteria release a toxin that affects the nerves, leading to muscle stiffness, spasm, or lockjaw. In serious cases, it can interfere with breathing and become life-threatening without treatment.
Diphtheria and pertussis are both respiratory infections that spread through coughing or sneezing, making them more contagious than tetanus. Diphtheria affects the nose and throat and, in more serious cases, can lead to breathing difficulties, heart problems, or nerve damage. Pertussis, more commonly known as whooping cough, causes severe coughing fits and can be especially dangerous for infants. Adults who are in close contact with babies — such as parents, grandparents, and caregivers — might unknowingly spread the illness if their vaccinations are not up to date.
This is why the Tdap booster remains an important part of adult health. While most people receive their initial doses in childhood, protection can fade over time. A booster is typically recommended every 10 years, or earlier depending on your age, lifestyle, travel plans, or medical history.
Who Should Get the Tdap Vaccine?
Adults who have never received a Tdap vaccine should get one, especially if it has been many years since their last tetanus shot. This recommendation becomes even more important for those who are in close contact with infants and young children.
Pregnant individuals are also advised to receive a Tdap vaccine during each pregnancy, ideally between weeks 27 and 36. This helps provide early protection for the newborn, who would otherwise be too young to receive their own vaccination.
How Often Should You Get the Tdap Vaccine?
If you’ve never received a Tdap vaccine as an adult, it might be time to go for one, even if you have completed your childhood vaccinations. Staying up to date is important for your own protection, especially if your lifestyle or environment puts you at higher risk of exposure.
In certain situations, another dose might be appropriate — for example, after a deep or contaminated wound, or based on your medical history. If you're unsure about when you were last vaccinated, speak to a doctor who can assess whether any follow-up is needed for your age, health, or lifestyle.
The HPV Vaccine – Key in Cancer Prevention
The human papillomavirus (HPV) is a virus that affects men and women. While many infections cause no symptoms and clear on their own, certain types are known to cause more serious complications — including cancers of the cervix, genital areas, and throat.
The HPV vaccine helps protect against these high-risk types. HPV types 16 and 18 are associated with cervical cancer, while types 6 and 11 are linked to the majority of genital warts. The vaccine targets these specific types to reduce the risk of both cancer and HPV-related growths.
There are also other types of HPV that might cause warts in non-genital areas, such as plantar warts on the soles of the feet. While these are unrelated to the types covered by the vaccine, they highlight just how widespread the HPV virus family can be.
In Singapore, the HPV vaccine is approved for individuals up to age 45. It remains an important way for adults to stay protected against HPV-related complications. While it might not always be top of mind, the price of putting it off can surface later — through preventable health issues or treatments that end up being more complex than expected.
Who Should Get the HPV Vaccine?
In Singapore, the HPV vaccine is approved for females and males aged nine to 45. It offers the greatest benefit when given before sexual activity begins, but adults can still gain important protection against certain HPV types.
Two vaccine types are available. The HPV2 targets HPV types 16 and 18, while HPV9 as its name indicates offers broader protection against nine HPV types, including those linked to genital warts and other cancers.
Based on individual health needs and doctor’s advice, females aged nine to 25 are eligible for either vaccine. For males and females up to age 45, the broader-spectrum option (HPV9) is generally preferred. If you're unsure, check with a doctor for advice.
How Often Should You Get the HPV Vaccine?
The HPV vaccine is not given yearly. Instead, it follows a fixed schedule based on your age and the type of vaccine used. Once the full course is completed, no booster is currently required.
There are two main vaccine types available in Singapore, and their schedules differ slightly:
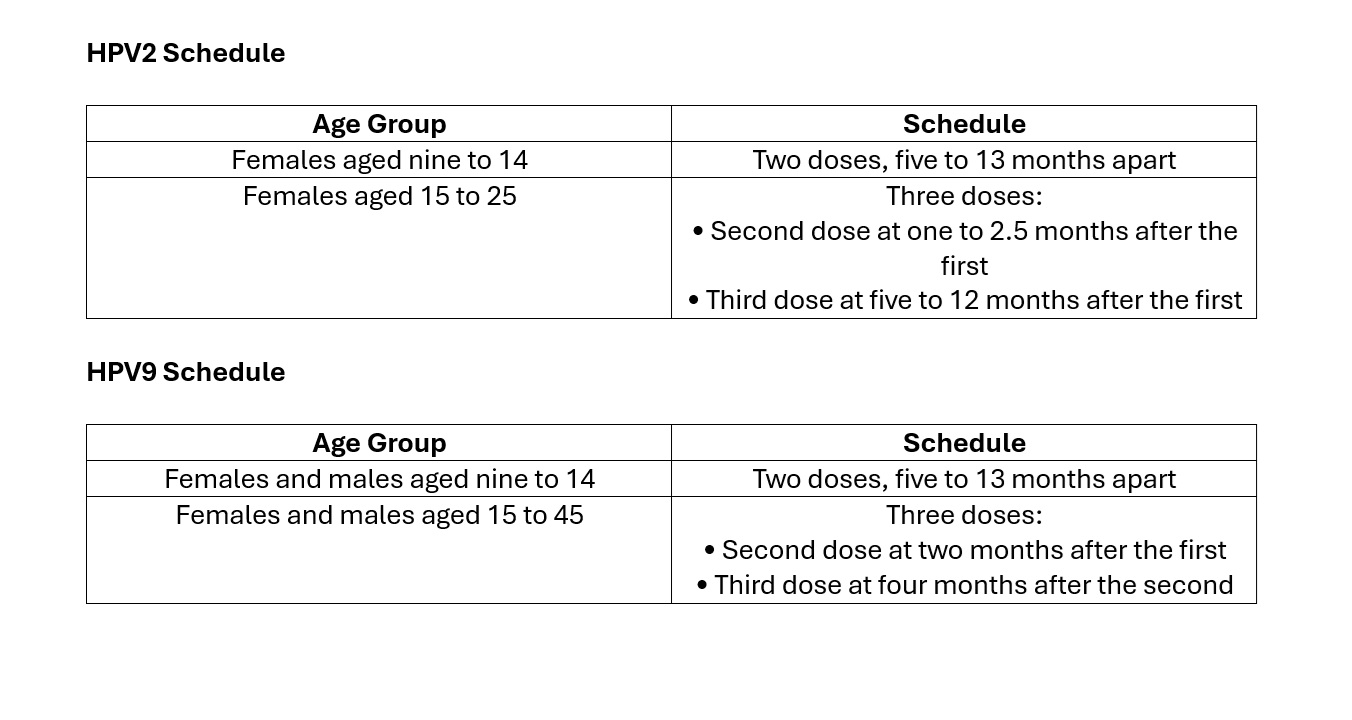
If you're unsure which HPV vaccine you received or how many doses you've had, a doctor can help confirm your records and advise on what’s next.
The MMR Vaccine – Why It Still Matters for Adults
The measles, mumps, and rubella (MMR) vaccine protects against three viral infections commonly associated with childhood. In Singapore, it forms part of the National Childhood Immunisation Schedule, with most children receiving their doses on time. However, that doesn’t mean the risk is gone. These viruses continue to circulate globally, and in a world where travel is common, imported cases can still surface in the community.
For adults who might not have completed their vaccinations or are unsure of their status, the risk remains. Measles can lead to pneumonia or brain inflammation. Mumps might cause swelling of the salivary glands, meningitis, or even affect fertility in men. Rubella is usually mild in adults, but if contracted during pregnancy, it can result in serious birth defects. What the MMR vaccine does is provide protection against all three viruses in one single shot.
Checking your vaccination status can still be relevant, especially if you're unsure whether you’ve received both doses. A quick conversation with your doctor can help clarify your records and assess whether any further action is needed.
Who Should Get the MMR Vaccine?
The MMR vaccine is recommended for adults who might not have completed the full two-dose series or are unsure of their vaccination history. This is particularly relevant in Singapore, where the rollout of measles and MMR vaccination evolved over time. The monovalent measles vaccine was introduced in 1976, made compulsory in 1985, and later replaced by the combined MMR vaccine in 1990. Because of this timeline, adults born in the 1970s and 1980s might not have received full coverage — making it important to check your vaccination status with a doctor.
How Often Should You Get the MMR Vaccine?
The MMR vaccine does not require yearly boosters. For most adults, completing the two-dose series is enough to provide long-term protection. If you've received only one dose, or aren't certain about your vaccination history, your doctor may recommend another dose for full coverage.
The Hepatitis B Vaccine – Still Important for Adults
Hepatitis B is a viral infection that targets the liver and can lead to serious consequences if left untreated. These include long-term complications like chronic hepatitis, cirrhosis, and liver cancer. The virus spreads through contact with infected blood or bodily fluids, which means it can be transmitted through shared personal items, unprotected sex, or even from mother to baby at birth. Although it may not always present symptoms, Hepatitis B can be silently damaging the liver before any signs appear.
Early signs, when they do show, might include jaundice, nausea, abdominal discomfort, or joint pain. However, many people carry the virus without knowing it, which makes vaccination an important form of protection for yourself and those around you. This is especially relevant for adults who might not have received the full series of vaccines in childhood, or who have risk factors linked to their work, lifestyle, or medical history.
In Singapore, the Hepatitis B vaccine is part of the National Childhood and National Adult Immunisation Schedules. It plays a key role in public health by reducing the spread of infection and protecting at-risk groups.
Who Should Get the Hepatitis B Vaccine?
The Hepatitis B vaccine is recommended for unvaccinated adults who may be at higher risk of infection. This includes:
- Healthcare workers and caregivers
- Individuals with a history of sexually transmitted infections
- Adults with chronic liver disease or kidney conditions
- Those living in close contact with someone who has Hepatitis B
- Travellers who are visiting countries where Hepatitis B is more common
Adults who have completed the vaccine series earlier in life but continue to face a higher risk are also advised to get a booster dose. If you're unsure whether you've been vaccinated or still have adequate protection, a simple blood test can help clarify your immunity status.
Important Note: The vaccine is not suitable for individuals with a known allergy to any component of the vaccine, including yeast, or those who have had a severe reaction to a previous dose. A doctor can advise on alternatives if needed.
How Often Should You Get the Hepatitis B Vaccine?
The standard Hepatitis B vaccination schedule involves three doses over six months:
- First dose: Chosen start date
- Second dose: One month after the first
- Third dose: Six months after the first
This series is typically given once in a lifetime. Once completed, most healthy adults do not require additional doses unless recommended by a doctor. In certain cases, a booster dose might be advised for those with weakened immune systems or ongoing exposure risks.
Unsure About Your Vaccination Status? Let’s Clear It Up!
Vaccine protection isn’t just for childhood. It continues to play an important role for adults, offering defence against infections that can lead to serious health issues later in life. Whether it's for work, travel, or everyday protection, staying updated on your vaccines is one of the simplest ways to care for your long-term health.
If it’s been a while since you last reviewed your vaccination history, now’s a good time to do so. You might be due for a follow-up dose or simply need clarity on what you’ve already received. A short conversation with a doctor can help confirm what’s next for your age, lifestyle, and health profile.
At Healthway Medical, we’re here to support you. If you’re looking for clear guidance or need help getting started, our clinics are ready to assist, so you can stay protected with confidence and peace of mind.





