Early Detection, Better Digestion: Benefits of Early Gastroparesis Screening
Content Outline
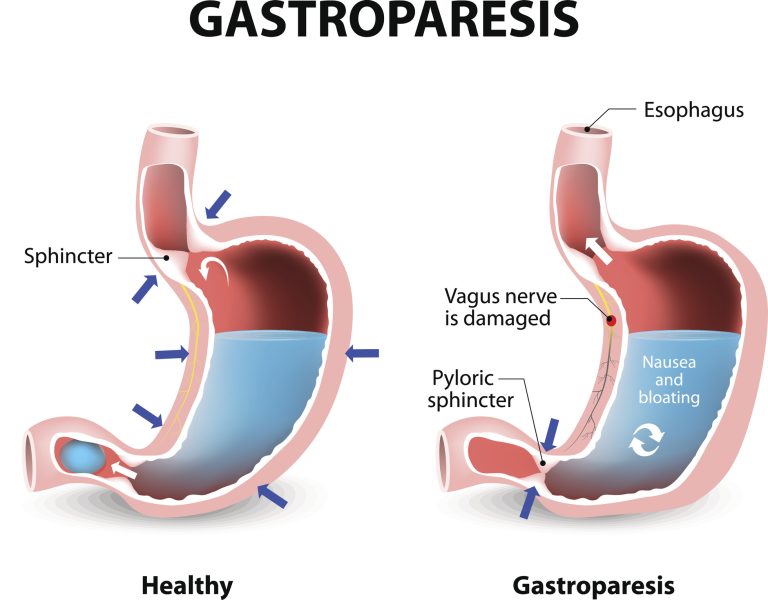
What Causes Gastroparesis?
This article explores how one can identify gastroparesis symptoms and obtain a diagnosis through a combination of health screening methods and diagnostic tests.
Recognising symptoms of Gastroparesis
Early identification of symptoms is vital for timely diagnosis and effective management. Here are some of the key symptoms:
- Nausea and Vomiting:
Persistent nausea is a common symptom, and vomiting may occur, especially after meals, often involving undigested food from previous meals.
- Early Satiety:
Individuals with gastroparesis will feel full after eating a small amount, which can lead to inadequate nutrition and unintended weight loss.
- Abdominal Pain and Bloating:
A feeling of fullness or bloating in the abdomen is common, causing discomfort and the sensation of being overly full.
- Acid Reflux:
Symptoms of heartburn or gastroesophageal reflux disease (GERD) may occur as food remains in the stomach longer than normal.
- Blood Sugar Fluctuations:
In individuals with diabetes, unpredictable gastric emptying can cause erratic blood sugar levels, complicating diabetes management
- Reduced Appetite:
Due to discomfort and a feeling of fullness, a decreased desire to eat is common, potentially leading to nutritional deficiencies.

Importance of Early Detection of Gastroparesis
One of the primary concerns is malnutrition, as delayed gastric emptying prevents the body from absorbing essential nutrients, leading to weight loss and deficiencies that can weaken overall health. This condition can also exacerbate underlying conditions, such as diabetes, making blood sugar management more challenging, increasing the risk of complications. Additionally, symptoms such as persistent vomiting associated with gastroparesis can cause dehydration and electrolyte imbalances, which, if not addressed promptly, can become life-threatening.
It is crucial to identify and manage gastroparesis early to prevent severe outcomes. In addition, early detection can provide benefits such as;
- Identifies Underlying Cause
Allows earlier treatment and prevention of complications, e.g. diabetes, which may be contributing to gastroparesis.
- Improves Quality of Life
Prompt treatment can alleviate debilitating symptoms like nausea, vomiting, and abdominal pain, enhancing patients’ daily functioning.
- Prevents Malnutrition
Implementing dietary modifications and nutritional support before malnutrition occurs.
Aiming to stay on top of your health goals?
offer a holistic approach to your health with comprehensive screening services.
What to do when experiencing these symptoms?
- Review Symptoms
Patients are asked about their symptoms, including the frequency and severity of nausea, vomiting, bloating, and abdominal pain. Understanding the impact of these symptoms on daily life is essential for diagnosis. - Assess Medical History
Doctors inquire about underlying health conditions, such as diabetes and neurological disorders, which can contribute to gastroparesis. They also review current medications and past surgeries that may affect gastric motility. - Perform a Physical Examination:
A physical exam helps to identify signs of dehydration, malnutrition, and abdominal abnormalities, which can provide clues to the presence of gastroparesis.

consult our friendly GPs at any Healthway Medical Clinics
Diagnostic Tests for Gastroparesis
1. Gastroscopy
Gastroscopy, also known as an upper gastrointestinal (GI) endoscopy, is a procedure that allows doctors to examine the lining of the upper digestive tract (oesophagus, stomach, and the first part of the small intestine). This procedure is performed using a thin, flexible tube called an endoscope, which has a tiny camera and light attached to its end. The procedure is invaluable for ruling out potential causes of digestive symptoms, such as an obstruction. Its ability to detect changes in the digestive lining can lead to the early identification of conditions, such as ulcers, and early-stage stomach cancers.